features
Cancer: Probability, Causes and Threat
What is Cancer?
Cancer is refers to a group of diseases involving abnormal cell growth with the potential to invade or spread to other parts of the body. They form a subset of neoplasm. A neoplasm or tumor is a group of cells that have undergone unregulated growth and will often form a mass or lump. But may be distributed diffusely.
However, the following features are common to all types of cancer:
· Abnormal cell growth
· Capacity to invade other tissues
· Capacity to spread to distant organs via blood vessels or lymphatic channels (metastasis)
If cancer is left untreated, it can invade tissues, spread through the body and eventually lead to death. The study of cancer is termed oncology. Cancers have been known to mankind since ancient times. Cancer begins when cells in a part of the body start to grow out of control. Several different parts of the body may be affected by cancer.
How does cancer occur?
The body is made up of trillions of cells that usually grow, divide and die in an organized manner. This process is a tightly controlled by the DNA machinery within the cell. When a person is developing and growing up, cells divide rapidly to allow for growth but once adulthood is reached, cells mainly only divide to replace worn-out or dying cells or to repair injuries.
Cancer occurs when cells in a particular site start to grow out of control. Rather than dying, they continue to grow and form new, abnormal cells. These abnormal cells can also invade other tissues, a property that normal cells do not possess.
Molecular pathology of cancer
Cancer cells originate from normal cells in which the DNA (deoxyribonucleic acid) within the cell nucleus has become damaged or mutated.
DNA is the “blueprint” contained in every cell that carries instructions for the cell’s function, growth, protein synthesis and death. When this DNA becomes damaged, the cell usually either repairs the damage or dies.
However, in cancer cells, the damaged DNA is not repaired and neither does the cell die. Instead, it gives rise to many more abnormal cells that all contain the same defective DNA as the original cancer cell.
Cancer; a History
Some of the earliest evidence of cancer is found among fossilized bone tumors in human mummies in ancient Egypt, and references to the same has been found in ancient manuscripts. Bony skull destruction as seen in cancer of the head and neck has been found, too.
Although the word cancer was not used, the oldest description of the disease is from Egypt and dates back to about 3000 BC. It is called the Edwin Smith Papyrus and is a copy of part of an ancient Egyptian textbook on trauma surgery. It describes 8 cases of tumors or ulcers of the breast that were treated by cauterization with a tool called the fire drill. The description adds that there is not treatment for the condition.
Origin of the word cancer
The disease was first called cancer by Greek physician Hippocrates (460-370 BC). He is considered the “Father of Medicine.” Hippocrates used the terms carcinos and carcinoma to describe non-ulcer forming and ulcer-forming tumors. In Greek this means a crab. The description was names after the crab because the finger-like spreading projections from a cancer called to mind the shape of a crab.Later Roman physician, Celsus (28-50 BC) translated the Greek term into cancer, the Latin word for crab. It was Galen (130-200 AD), another Roman physician, who used the term oncos (Greek for swelling) to describe tumors. Oncos is the root word for oncology or study of cancers.
Between 15th and 18th centuries
During the beginning of the 15th Century scientists developed greater understanding of the workings of human body and its disease processes. Autopsies, done by Harvey (1628), led to an understanding of the circulation of blood through the heart and body. Giovanni Morgagni of Padua in 1761 regularized autopsies to find the cause of diseases. This laid the foundation for the study of cancer as well.
It was Scottish surgeon John Hunter (1728−1793) who suggested that some cancers might be cured by surgery. It was nearly a century later that development of anesthesia prompted regular surgery for “movable” cancers that had not spread to other organs.
The 19th Century
Rudolf Virchow, often called the founder of cellular pathology, founded the basis for pathologic study of cancers under the microscope. Virchow correlated microscopic pathology to illness. He also developed study of tissues that were taken out after surgery. The pathologist could also tell the surgeon whether the operation had completely removed the cancer.
History of the causes of cancer
There have been numerous theories of causes of cancer throughout ages. For example, the ancient Egyptians blamed Gods for cancers.
· Hippocrates believed that the body had 4 humors (body fluids): blood, phlegm, yellow bile, and black bile. He suggested that an imbalance of these humors with an excess of black bile in various body sites could cause cancer. This was the humoral theory.
· After the humoral theory came the lymph theory. Stahl and Hoffman theorized that cancer was composed of fermenting and degenerating lymph, varying in density, acidity, and alkalinity. John Hunter, the Scottish surgeon from the 1700s, agreed that tumors grow from lymph constantly released from blood.
· Zacutus Lusitani (1575−1642) and Nicholas Tulp (1593−1674), doctors in Holland, concluded that cancer was contagious. Throughout the 17th and 18th centuries, some believed that cancer was contagious.
· It was it 1838 that German pathologist Johannes Muller showed that cancer is made up of cells rather than lymph. Muller proposed that cancer cells developed from budding elements (blastema) between normal tissues.
· Rudolph Virchow (1821−1902), suggested that all cells, including cancer cells, are derived from other cells. He proposed the chronic irritation theory. He believed that cancer spread like a liquid. In the 1860s, German surgeon, Karl Thiersch, showed that cancers metastasize through the spread of malignant cells and not through a liquid.
· Until 1920’s trauma was thought to be the cause of cancers.
Now a day,the majority of cancers, some 90–95% of cases, are due to environmental factors. The remaining 5–10% are due to inherited genetics. Environmental, as used by cancer researchers, means any cause that is not inherited genetically, such as lifestyle, economic and behavioral factors and not merely pollution. Common environmental factors that contribute to cancer death include tobacco (25–30%), diet and obesity (30–35%), infections (15–20%), radiation (both ionizing and non-ionizing, up to 10%), stress, lack of physical activity and pollution.
It is not generally possible to prove what caused a particular cancer because the various causes do not have specific fingerprints. For example, if a person who uses tobacco heavily develops lung cancer, then it was probably caused by the tobacco use, but since everyone has a small chance of developing lung cancer as a result of air pollution or radiation, the cancer may have developed for one of those reasons. Excepting the rare transmissions that occur with pregnancies and occasional organ donors, cancer is generally not a transmissible disease.
History of cancer screening and detection
Screening for cancer helps in early detection. The first screening test to be widely used for cancer was the Pap test. It was developed by George Papanicolaou as a research method in understanding the menstrual cycle. He then noted that the test could help in finding cervical cancer early and presented his findings in 1923.It was then that the American Cancer Society (ACS) promoted the test during the early 1960’s and it became widely used as a screening tool.Modern mammography methods were developed late in the 1960’s and first officially recommended for breast cancer screening by the ACS in 1976.
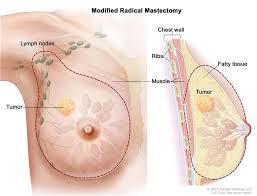
Development of cancer surgery
It was quite early in the history of knowledge of cancers that surgery was considered a modality of treatment of cancers. Roman physician Celsus had noted that despite surgery the cancer seems to come back. Galen wrote about techniques of surgery for cancers. Surgery then was very primitive with many complications, including blood loss. Surgery for cancers flourished in the 19th and early 20th centuries after advancement of anesthesia.
Bilroth in Germany, Handley in London, and Halsted in Baltimore are the pioneers of cancer surgery. William Stewart Halsted, professor of surgery at Johns Hopkins University, developed the radical mastectomy during the last decade of the 19th century for breast cancers. His work was based on W. Sampson Handley.
Stephen Paget, an English surgeon during this time found that cancers did spread via blood circulation. This understanding of metastasis became a key element in recognizing patients who might and might not benefit from cancer surgery.
Development of radiation therapy
In 1896 a German physics professor, Wilhelm Conrad Roentgen, discovered and presented the properties of X rays. It was within the next few months that X rays were used for diagnosis and in the next 3 years it was used in treatment of cancers. Radiation therapy began with radium and with relatively low-voltage diagnostic machines.
Development of chemotherapy
It was seen that during the World War II, soldiers exposed to mustard gas during military action developed toxic bone marrow suppression. Soon a similar chemical nitrogen mustard was found to work against a cancer of the lymph nodes called lymphoma. This laid foundation for several new drugs that could be used against cancers.
Development of hormone therapy
In the 19th Century, Thomas Beatson discovered that the breasts of rabbits stopped producing milk after he removed the ovaries. He tried removal of the ovaries (called oophorectomy) in advanced breast cancer. This was discovered before the hormone itself was discovered. His work provided a foundation for the modern use of hormone therapy, such as tamoxifen and the aromatase inhibitors, to treat or prevent breast cancer.
Development of immunotherapy
With the understanding of the biology of cancer cells, several biological agents have been developed in treatment of cancers. These are called biological response modifier (BRM) therapy. Notable among these are the monoclonal antibodies.
The first therapeutic monoclonal antibodies, rituximab (Rituxan) and trastuzumab (Herceptin) were approved during the late 1990’s to treat lymphoma and breast cancer, respectively. Scientists are also studying vaccines that boost the body’s immune response to cancer cells.
The later part of the 20th century also saw the development of targeted therapies like growth factor inhibitors like trastuzumab (Herceptin), gefitinib (Iressa), imatinib (Gleevec), and cetuximab (Erbitux). Another targeted approach is anti- ngiogenesis or anti-blood vessel formation drugs like bevacizumab (Avastin).
DNA damage may be inherited or it may occur spontaneously at any point in a person’s life. DNA damage can be triggered by exposure to certain toxins such as those present in cigarette smoke, for example. There are, however, multiple factors that can cause cancer and it is often difficult to pinpoint an exact cause.
Tumors
As cancer cells proliferate, they eventually form tumors. Not all tumors are cancerous and capable of spreading. Those that are capable of spreading are referred to as malignant tumors. Benign tumors, on the other hand, do not invade other organs or spread to other parts of the body, although they can grow to a large size and start to press on surrounding organs and tissues.
Who gets cancer and how common is cancer?
There are millions of people worldwide who are living with cancer or have had cancer. Estimates suggest that around half of all American men and one third of all American women will develop cancer during their lifetimes. Healthy lifestyle factors can be adopted to help reduce the risk of cancer such as taking regular physical activity, maintaining a healthy diet and body weight and avoiding known risk factors such as exposure to tobacco smoke and too much sunbathing.
For some common cancers such as breast cancer and colon cancer, effective screening tests are available to help detect the disease as early on as possible. Early diagnosis and treatment initiation often improves the chance of a good response to anti-cancer therapy and therefore recovery.
Here are several terms that are used in context of cancer. Some of these include:
Terms related to cancer types
· Tumor or tumour – this means any abnormal swelling, lump or mass.
· Neoplasm – this is the medical term for cancer and is synonymous with it.
· Neoplasm may be further spoken of as a malignant neoplasm or cancer.
· Benign neoplasm or benign tumor.
· An invasive tumor is one that signifies the invasiveness of the cancer.
· A non-invasive tumor is one that is not yet invasive but has the potential to turn aggressive and invade other organs.
· Atypia, dysplasia and carcinoma in situ – this is a form of non invasive tumors where the cells begin to show abnormality under the microscope.
· Carcinoma – this is a type of cancer that begins in the skin or in tissues that line or cover internal organs.
· Sarcoma – this type of cancer begins in bone, cartilage, fat, muscle, blood vessels and other supportive tissues.
· Leukemia – this type of cancer starts in blood-forming tissue such as the bone marrow leading to production of large numbers of abnormal blood cells - this is called blood cancer is common parlance.
· Lymphoma and myeloma – these are cancers that begin in the cells of the immune system.
Terms related to diagnosis and pathology of cancer
· Screening – this refers to a test that is done routinely at fixed age and intervals among healthy persons to detect tumors before they become apparent. A good example of a screening test is a mammogram to detect breast cancer. These tests are usually minimally painful or invasive to increase their acceptability.
· Biopsy – this is a laboratory test that involves removal of a sample of tissues from a cancer or tumor to check the cells under the microscope for abnormality. There are several types of biopsy procedures like fine needle aspiration, core biopsy or excision biopsy.
· Grade of the tumor – This is usually defined as the degree of resemblance of the tumor to the surrounding benign tissue. A low grade tumor resembles the surrounding normal tissues closely while a high grade tumor is very different from surrounding tissues. An intermediate grade lies somewhere in between.
· Stage of cancer – This is usually a number (usually between 0 to 4) that describe the degree of invasion of the body by the tumor. A grade 4 cancer is an advanced cancer that has spread to distant organs and is less amenable to treatment.
· Metastasis – Spread of tumors to distant sites away from the original site of the cancer.
· Transformation of the tumor – This refers to change of a low grade tumor to a high grade tumor.
· Aggressive tumor – a minimally aggressive tumor spreads slowly whereas an aggressive tumor tends to spread faster.
· Oncologist – a Specialist who deals with cancer and its treatment.
· An oncopatholgist – a pathologist who helps in diagnosis and detection of cancers.
Kinds of tumor marker
ALK gene rearrangements and overexpression
· Cancer types: Non-small cell lung cancer and anaplastic large cell lymphoma
· Tissue analyzed: Tumor
· How used: To help determine treatment and prognosis
Alpha-fetoprotein (AFP)
· Cancer types: Liver cancer and germ cell tumors
· Tissue analyzed: Blood
· How used: To help diagnose liver cancer and follow response to treatment; to assess stage, prognosis, and response to treatment of germ cell tumors
Beta-2-microglobulin (B2M)
· Cancer types: Multiple myeloma, chronic lymphocytic leukemia, and some lymphomas
· Tissue analyzed: Blood, urine, or cerebrospinal fluid
· How used: To determine prognosis and follow response to treatment
Beta-human chorionic gonadotropin (Beta-hCG)
· Cancer types: Choriocarcinoma and germ cell tumors
· Tissue analyzed: Urine or blood
· How used: To assess stage, prognosis, and response to treatment
BRCA1 and BRCA2 gene mutations
· Cancer type: Ovarian cancer
· Tissue analyzed: Blood
· How used: To determine whether treatment with a particular type of targeted therapy is appropriate
BCR-ABL fusion gene (Philadelphia chromosome)
· Cancer type: Chronic myeloid leukemia, acute lymphoblastic leukemia, and acute myelogenous leukemia
· Tissue analyzed: Blood and/or bone marrow
· How used: To confirm diagnosis, predict response to targeted therapy, and monitor disease status
BRAF V600 mutations
· Cancer types: Cutaneous melanoma and colorectal cancer
· Tissue analyzed: Tumor
· How used: To select patients who are most likely to benefit from treatment with certain targeted therapies
· Cancer types: Gastrointestinal stromal tumor and mucosal melanoma
· Tissue analyzed: Tumor
· How used: To help in diagnosing and determining treatment
CA15-3/CA27.29
· Cancer type: Breast cancer
· Tissue analyzed: Blood
· How used: To assess whether treatment is working or disease has recurred
CA19-9
· Cancer types: Pancreatic cancer, gallbladder cancer, bile duct cancer, and gastric cancer
· Tissue analyzed: Blood
· How used: To assess whether treatment is working
· Cancer type: Ovarian cancer
· Tissue analyzed: Blood
· How used: To help in diagnosis, assessment of response to treatment, and evaluation of recurrence
· Cancer type: Medullary thyroid cancer
· Tissue analyzed: Blood
· How used: To aid in diagnosis, check whether treatment is working, and assess recurrence
Carcinoembryonic antigen (CEA)
· Cancer types: Colorectal cancer and some other cancers
· Tissue analyzed: Blood
· How used: To keep track of how well cancer treatments are working or check if cancer has come back
· Cancer type: Non-Hodgkin lymphoma
· Tissue analyzed: Blood
· How used: To determine whether treatment with a targeted therapy is appropriate
Chromogranin A (CgA)
· Cancer type: Neuroendocrine tumors
· Tissue analyzed: Blood
· How used: To help in diagnosis, assessment of treatment response, and evaluation of recurrence
Chromosomes 3, 7, 17, and 9p21
· Cancer type: Bladder cancer
· Tissue analyzed: Urine
· How used: To help in monitoring for tumor recurrence
Circulating tumor cells of epithelial origin (CELLSEARCH®)
· Cancer types: Metastatic breast, prostate, and colorectal cancers
· Tissue analyzed: Blood
· How used: To inform clinical decision making, and to assess prognosis
Cytokeratin fragment 21-1
· Cancer type: Lung cancer
· Tissue analyzed: Blood
· How used: To help in monitoring for recurrence
EGFR gene mutation analysis
· Cancer type: Non-small cell lung cancer
· Tissue analyzed: Tumor
· How used: To help determine treatment and prognosis
Estrogen receptor (ER)/progesterone receptor (PR)
· Cancer type: Breast cancer
· Tissue analyzed: Tumor
· How used: To determine whether treatment with hormone therapy and some targeted therapies is appropriate
Fibrin/fibrinogen
· Cancer type: Bladder cancer
· Tissue analyzed: Urine
· How used: To monitor progression and response to treatment
· Cancer type: Ovarian cancer
· Tissue analyzed: Blood
· How used: To plan cancer treatment, assess disease progression, and monitor for recurrence
HER2/neu gene amplification or protein overexpression
· Cancer types: Breast cancer, gastric cancer, and gastroesophageal junction adenocarcinoma
· Tissue analyzed: Tumor
· How used: To determine whether treatment with certain targeted therapies is appropriate
Immunoglobulins
· Cancer types: Multiple myeloma and Waldenström macroglobulinemia
· Tissue analyzed: Blood and urine
· How used: To help diagnose disease, assess response to treatment, and look for recurrence
KRAS gene mutation analysis
· Cancer types: Colorectal cancer and non-small cell lung cancer
· Tissue analyzed: Tumor
· How used: To determine whether treatment with a particular type of targeted therapy is appropriate
· Cancer types: Germ cell tumors, lymphoma, leukemia, melanoma, and neuroblastoma
· Tissue analyzed: Blood
· How used: To assess stage, prognosis, and response to treatment
Neuron-specific enolase (NSE)
· Cancer types: Small cell lung cancer and neuroblastoma
· Tissue analyzed: Blood
· How used: To help in diagnosis and to assess response to treatment
Nuclear matrix protein 22
· Cancer type: Bladder cancer
· Tissue analyzed: Urine
· How used: To monitor response to treatment
Programmed death ligand 1 (PD-L1)
· Cancer type: Non-small cell lung cancer
· Tissue analyzed: Tumor
· How used: To determine whether treatment with a particular type of targeted therapy is appropriate
Prostate-specific antigen (PSA)
· Cancer type: Prostate cancer
· Tissue analyzed: Blood
· How used: To help in diagnosis, assess response to treatment, and look for recurrence
· Cancer type: Thyroid cancer
· Tissue analyzed: Blood
· How used: To evaluate response to treatment and look for recurrence
Urokinase plasminogen activator (uPA) and plasminogen activator inhibitor (PAI-1)
· Cancer type: Breast cancer
· Tissue analyzed: Tumor
· How used: To determine aggressiveness of cancer and guide treatment
5-Protein signature (OVA1®)
· Cancer type: Ovarian cancer
· Tissue analyzed: Blood
· How used: To pre-operatively assess pelvic mass for suspected ovarian cancer
21-Gene signature (Oncotype DX®)
· Cancer type: Breast cancer
· Tissue analyzed: Tumor
· How used: To evaluate risk of recurrence
70-Gene signature (Mammaprint®)
· Cancer type: Breast cancer
· Tissue analyzed: Tumor
· How used: To evaluate risk of recurrence
Terms related to treatment of cancer
Related Stories
· Large NIH grant awarded to Dartmouth researchers for cooperative lung cancer project
· Study uncovers new genetic variants for lung cancer risk
· Combination therapy may lead to new standard of care for kidney cancer patients
· Remission – when a cancer patient shows no sign of cancer after therapy, he or she is said to be in remission. They are kept under a close watch and system of monitoring and follow up to detect a relapse.
· Cure – a cure is considered in a cancer patient if 95% of treated patients live a certain period of time after the date of their diagnosis of cancer. For Hodgkin’s lymphoma it is 10 years, whereas for Burkitt's lymphoma this period is 1 year.
· Recurrence – if the cancer returns at the site of the original tumor after surgery or treatment, it is called a recurrence.
· Median survival time – this is a period of time measured in months or years over which at least 50% of the cancer patients are expected to be alive.
· Overall survival – this is statistical term that determines the maximum survivability with a cancer.
· Prognosis – this is the possible outcome of a cancer. It is usually expressed as a probability of survival five years after diagnosis. It can also be expressed as the number of years when 50% of the patients are still alive. A graphical analysis by the Kaplan-Meier curve is used to determine the prognosis.
· Protocol – This refers to the specific chemotherapy plan that is used.
· Chemotherapy – this refers to the treatment of cancer using anti-cancer drugs.
· Cycle - chemotherapy drugs are often given in the same order on the same schedule repeatedly. These are called cycles of chemotherapy.
· Radiation therapy – this treatment refers to therapy with high energy beams or rays and radiation to kill the cancer cells.
· Adjuvant therapy – this is usually given with chemotherapy or radiation therapy. This is given after surgery to kill the remaining cancer cells.
· Neo-adjuvant therapy – This is similar to adjuvant therapy used before surgery to reduce the burden of cancer cells.
· Palliative therapy – This refers to symptomatic relief that is provided in patients with advanced cancers.
Cancers may be classified by their primary site of origin or by their histological or tissue types.
Classification by site of origin
By primary site of origin, cancers may be of specific types like breast cancer, lung cancer, prostate cancer, liver cancer renal cell carcinoma (kidney cancer), oral cancer, brain cancer etc.
Classification by tissue types
The international standard for the classification and nomenclature of histologies is the International Classification of Diseases for Oncology, Third Edition (ICD-O-3). This classification is based on the ICD-O-3.
Based on tissue types cancers may be classified into six major categories:
1. Carcinoma
This type of cancer originates from the epithelial layer of cells that form the lining of external parts of the body or the internal linings of organs within the body.
Carcinomas, malignancies of epithelial tissue, account for 80 to 90 percent of all cancer cases since epithelial tissues are most abundantly found in the body from being present in the skin to the covering and lining of organs and internal passageways, such as the gastrointestinal tract.Carcinomas usually affect organs or glands capable of secretion including breast, lungs, bladder, colon and prostate.
Carcinomas are of two types – adenocarcinoma and squamous cell carcinoma. Adenocarcinoma develops in an organ or gland and squamous cell carcinoma originates in squamous epithelium. Adenocarcinomas may affect mucus membranes and are first seen as a thickened plaque-like white mucosa. These are rapidly spreading cancers.
2. Sarcoma
These cancers originate in connective and supportive tissues including muscles, bones, cartilage and fat. Bone cancer is one of the sarcomas termed osteosarcoma. It affects the young most commonly. Sarcomas appear like the tissue in which they grow.
Other examples include chondrosarcoma (of the cartilage), leiomyosarcoma (smooth muscles), rhabdomyosarcoma (skeletal muscles), Mesothelial sarcoma or mesothelioma (membranous lining of body cavities), Fibrosarcoma (fibrous tissue), Angiosarcoma or hemangioendothelioma (blood vessels), Liposarcoma (adipose or fatty tissue), Glioma or astrocytoma (neurogenic connective tissue found in the brain), Myxosarcoma (primitive embryonic connective tissue) and Mesenchymous or mixed mesodermal tumor (mixed connective tissue types).
3. Myeloma
These originate in the plasma cells of bone marrow. Plasma cells are capable of producing various antibodies in response to infections. Myeloma is a type of blood cancer.
4. Leukemia
This group of cancers that are grouped within blood cancers. These cancers affect the bone marrow which is the site for blood cell production. When cancerous, the bone marrow begins to produce excessive immature white blood cells that fail to perform their usual actions and the patient is often prone to infection.
Types of leukemia include:
· Acute myelocytic leukemia (AML) – these are malignancy of the myeloid and granulocytic white blood cell series seen in childhood.
· Chronic myelocytic leukemia (CML) – this is seen in adulthood.
· Acute Lymphatic, lymphocytic, or lymphoblastic leukemia (ALL) – these are malignancy of the lymphoid and lymphocytic blood cell series seen in childhood and young adults.
· Chronic Lymphatic, lymphocytic, or lymphoblastic leukemia (CLL) – this is seen in the elderly.
· Polycythemia vera or erythremia – this is cancer of various blood cell products with a predominance of red blood cells.
5. Lymphoma
Related Stories
· Scientists develop potential new therapy for targeting skin cancer metastases in the brain
· Cancer diagnosis now more common than marriage, says MacMillan Cancer Support
· Pre-existing illness delays bowel cancer diagnosis
These are cancers of the lymphatic system. Unlike the leukemias, which affect the blood and are called “liquid cancers”, lymphomas are “solid cancers”. These may affect lymph nodes at specific sites like stomach, brain, intestines etc. These lymphomas are referred to as extranodal lymphomas.
Lymphomas may be of two types – Hodgkin’s lymphoma and Non-Hodgkin’s lymphomas. In Hodgkin lymphoma there is characteristic presence of Reed-Sternberg cells in the tissue samples which are not present in Non-Hodgkin lymphoma.
6. Mixed types
These have two or more components of the cancer. Some of the examples include mixed mesodermal tumor, carcinosarcoma, adenosquamous carcinoma and teratocarcinoma. Blastomas are another type that involves embryonic tissues.
Classification by grade
Cancers can also be classified according to grade. The abnormality of the cells with respect to surrounding normal tissues determines the grade of the cancer. Increasing abnormality increases the grade, from 1–4.
Cells that are well differentiated closely resemble normal specialized cells and belong to low grade tumors. Cells that are undifferentiated are highly abnormal with respect to surrounding tissues. These are high grade tumors.
· Grade 1 – well differentiated cells with slight abnormality
· Grade 2 – cells are moderately differentiated and slightly more abnormal
· Grade 3 – cells are poorly differentiated and very abnormal
· Grade 4 – cells are immature and primitive and undifferentiated
Classification by stage
Cancers are also classified individually according to their stage. There are several types of staging methods. The most commonly used method uses classification in terms of tumor size (T), the degree of regional spread or node involvement (N), and distant metastasis (M). This is called the TNM staging.
For example, T0 signifies no evidence of tumor, T 1 to 4 signifies increasing tumor size and involvement and Tis signifies carcinoma in situ or limited to surface cells. Similarly N0 signifies no nodal involvement and N 1 to 4 signifies increasing degrees of lymph node involvement. Nx signifies that node involvement cannot be assessed. Metastasis is further classified into two – M0 signifies no evidence of distant spread while M1 signifies evidence of distant spread.
Stages may be divided according to the TNM staging classification. Stage 0 indicates cancer being in situ or limited to surface cells while stage I indicates cancer being limited to the tissue of origin. Stage II indicates limited local spread, Stage II indicates extensive local and regional spread while stage IV is advanced cancer with distant spread and metastasis.
Cancer Symptoms
Cancers are a group of hundreds of different diseases and affect various organs of the body. Cancer symptoms depend on the stage of cancer, the grade of cancer, whether it has spread to other organs, the general health, age and condition of the patient and numerous other factors.
Types of cancer symptom
Broadly the symptoms of cancer can be divided into the following groups:
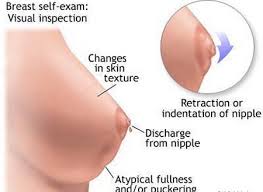
Local symptoms
This includes the symptoms at the primary site of cancer. This may be a lump or tumor, pain, bleeding, ulcers or sores over the skin, pressure over the surrounding organs, hoarseness or cough that does not go away, obvious changes in a wart or a mole, changes in bladder or bowel habits, difficulty in swallowing etc.
Systemic symptoms
This includes symptoms of the generalized body as a whole. Most of these are common for all types of cancer. These include weight loss, poor appetite, fatigue and wasting (known as cancer cachexia), excessive sweating especially at nights (night sweats), hormonal changes, anemia, bleeding tendencies due to deficiency of platelets (thrombocytopenia) etc.
Symptoms of spread of cancer or metastasis
This includes swelling of the nearing lymph nodes, cough, bleeding on coughing or hemoptysis (as seen in spread of the cancer to lungs), bone pain (as seen in spread of the cancer to bones), convulsions and neurological symptoms (as seen in spread of the cancer to brain), jaundice and abnormal liver function tests (as seen in spread of the cancer to liver) etc.It is important to know that these symptoms do not mean that the patient has cancer.
Pain, depression and fatigue
Pain, depression, and fatigue are prominent contributors to suffering of many cancer patients. Every year, cancer kills of severely debilitates millions of people worldwide. Symptoms such as depression, fatigue and cancer pain are often difficult to measure and quantify.
Cancer is related with intractable and severe pain. This may be acute, chronic or tumor-specific pain or related to treatment of procedure. Pain is a major cause of impaired quality of life in patients with cancer, and intensifies the distress and suffering. Inflammatory mediators associated with cancer include prostaglandins, cytokines, tumor necrosis factors, interleukins, growth factors and other tumor-derived chemicals that are known to cause pain. Pain may also occur due to the pressure applied by the cancer on surrounding organs.
General symptoms
· Fatigue · Pain · Loss of appetite or anorexia · Weight loss
Gastrointestinal system symptoms
· Difficulty in swallowing · Tastelessness · Feeling full · Excessive burping
· Excessive hiccupping · Mouth ulcers and sores · Nausea and vomiting
· Diarrhea · Constipation · Abdominal bloating
Respiratory system symptoms
· in sputum or hemoptysis · Hoarseness of Difficulty in breathing or shortness of breath
· Cough with excessive sputum · Blood voice
Cardio-vascular system symptoms
· Edema or swelling of face and feet · Palpitations
Neurological symptoms
· Insomnia or difficulty in sleeping · Excessive sleep · Distress · Depression
· Forgetfulness · Anxiety · Numbness or paralysis · Deafness · Blindness
Skin related symptoms
· Itching · Dry skin · Sores or ulcers that do not heal · Abnormal changes in warts or moles
Urological and genital symptoms
· Pain or difficulty in urination · Difficulty in holding in urine (incontinence)
· Pain and itching in the vagina (vaginitis) · Amenorrhea or absence of menstrual periods · Pain over the genital region (dyspareunia) · Loss of libido · Unnatural bleeding and spotting even after menopause · Impotence in males
What Causes Cancer?
Cancers are a broad group of diseases and accordingly have a wide range of causes. Each cancer is different according to its biology and pathophysiology. All animals and even plants are susceptible to cancers.
Cancer at the molecular level
The body is made up of trillions of living cells. These cells grow, divide, and die in an orderly fashion. This process is tightly regulated and is controlled by the DNA machinery within the cell. In a baby or a child normal cells divide rapidly to allow for growth. After the person becomes an adult, most cells divide only to replace worn-out or dying cells or to repair injuries.
When cells of the body at a particular site start to grow out of control, they may become cancerous. Cancer cell growth is different from normal cell growth. Instead of dying, cancer cells continue to grow and form new, abnormal cells. In addition, these cells can also invade other tissues. This is a property that normal cells do not possess.
Cancer cells originate from normal cells when their DNA (deoxyribonucleic acid) or blue prints within the cell nucleus is damaged. DNA is in every cell and it directs all the cell’s actions, growth, death, protein synthesis etc. when DNA is damaged in a normal cell the cell either repairs the damage or the cell dies.
Normally, the body safeguards against cancer via numerous methods, such as: apoptosis or a process by which abnormal cells die on their own accord, helper molecules (some DNA polymerases), possibly senescence or aging, etc.
In cancer cells, the damaged DNA is not repaired, and the cell does not die. Instead it gives rise to more such abnormal cells with abnormal DNA. These new cells all have the same defective DNA of the original cancer cell.
DNA damage may be inherited from parents or may be a spontaneous problem that occurs during the lifetime of a person. This is called a mutation. DNA damage may also be triggered by exposure to certain environmental toxins such as those present in cigarette smoke. There are, however, multiple factors that may cause cancer and it is difficult to pin point an exact cause.
Mutations
Mutations may be:
· Those in the error-correcting machinery of a cell. This may cause accumulation of errors rapidly in the cell and its progeny.
· Those in signaling (endocrine) machinery of the cell. This leads transmission of the error signals to nearby healthy cells as well.
· Those that allow the cells to migrate and disrupt more healthy cells away from the primary site of origin.
· Those that make the cell immortal so that the abnormal cell refuses to die.
Risk factors for cancer
According to World Health Organization (WHO), common risk factors for cancer include:
· Tobacco use
· Alcohol use
· Overweight and obesity
· Dietary factors, including insufficient fruit and vegetable intake
· Physical inactivity
· Chronic infections from helicobacter pylori, hepatitis B virus (HBV), hepatitis C virus (HCV) and some types of human papilloma virus (HPV)
· Environmental and occupational risks including ionizing and non-ionizing radiation
Cancer-causing agents
Agents that may cause cancer include:
Chemical carcinogens
Several chemicals and environmental toxins are responsible for changes in normal cellular DNA. Substances that cause DNA mutations are known as mutagens, and mutagens that cause cancers are known as carcinogens.
Particular substances have been linked to specific types of cancer. Tobacco smoking is associated with many forms of cancer, and causes 90% of lung cancer. Similarly, prolonged exposure to asbestos fibers is associated with mesothelioma.
Tobacco is also related to other cancers such as lung, larynx, head, neck, stomach, bladder, kidney, oesophagus and pancreas as it contains other known carcinogens, including nitrosamines and polycyclic aromatic hydrocarbons.
Ionizing radiations
Radiations due to radon gas and prolonged exposure to ultraviolet radiation from the sun can lead to melanoma and other skin malignancies. Radiation therapy given for one type of cancer may also cause another type of cancer. For example, those who receive chest radiation therapy for lymphomas may later develop breast cancer.
Viral and bacterial infections
Some cancers can be caused by infections with pathogens. Notable among these include liver cancers due to Hepatitic B and C infections; cervical cancer due to infections with Human Papilloma virus (HPV); Epstein Barr virus causing Burkitt’s lymphoma and gastric or stomach cancer due to Helicobacter pylori infection.
Genetic or inherited cancers
Common examples are inherited breast cancer and ovarian cancer genes including BRCA1 and 2. Li-Fraumeni syndrome includes defects in the p53 gene that leads to bone cancers, breast cancers, soft tissue sarcomas, brain cancers etc. Those with Down’s syndrome are known to develop malignancies such as leukemia and testicular cancer.
Hormonal changes
Notable among these are changes in the female hormone levels estrogen. Excess estrogen promotes uterine cancer.
Immune system dysfunction
Impaired immunity including HIV infection leads to several cancers including Kaposi's sarcoma, non-Hodgkin's lymphoma, and HPV-associated malignancies such as anal cancer and cervical cancer.
Cancer Pathophysiology
Cancer has a complex Pathophysiology. Pathologists are physicians who are concerned primarily with the study of disease in all its aspects. This includes cause of the disease, diagnosis, how the disease develops (pathogenesis), mechanism and natural course of the disease. They also deal with biochemical features, progression, and prognosis or outcome of the disease.
Pathology of cancers and other complex disorders have undergone a sea change after development of technologies like immunohistochemistry, flow cytometry, and molecular biologic approaches to cancer diagnosis.
Genetic changes
In normal cells, genes regulate growth, maturity and death of the cells. Genetic changes can occur at many levels. There could be a gain or loss of entire chromosomes or a single point mutation affecting a single DNA nucleotide.
There are two broad categories of genes which are affected by these change:
· Oncogenes – these are cancer causing genes. They may be normal genes which are expressed at inappropriately high levels in patients with cancers or they may be altered or changed normal genes due to mutation. In both cases these genes lead to cancerous changes in the tissues.
· Tumor suppressor genes – these genes normally inhibit cell division and prevent survival of cells that have damaged DNA. In patients with cancer these tumor suppressor genes are often disabled. This is caused by cancer-promoting genetic changes. Typically, changes in many genes are required to transform a normal cell into a cancer cell.
Genomic amplification
Sometimes there may be genomic amplification. Here a cell gains many copies (often 20 or more) of a small chromosomal locus, usually containing one or more oncogenes and adjacent genetic material.
Point mutations
Point mutations occur at single nucleotides. There may be deletions, and insertions especially at the promoter region of the gene. This changes the protein coded for by the particular gene. Disruption of a single gene may also result from integration of genomic material from a DNA virus or retrovirus. This may lead to formation of Oncogenes.
Translocation
Translocation is yet another process when two separate chromosomal regions become abnormally fused, often at a characteristic location. A common example is Philadelphia chromosome, or translocation of chromosomes 9 and 22, which occurs in chronic myelogenous leukaemia, and results in production of the BCR-abl fusion protein, an oncogenic tyrosine kinase.
Tumors
A tumor in Latin means a swelling but not all swellings are tumors in the modern sense of the term. Some of them may be caused due to inflammation, infections, cysts or fluid filled lesions or due to benign growths. A cancerous tumor has the capacity to grow rapidly and to metastasize or spread to other tissues. Some tumors like leukemia’s grow as cell suspensions but most grow as solid masses of tissue.
Solid tumor parts
Solid tumors have two distinct parts. One of them is the parenchyma that contains cancer tissues and cells and the other is the stroma that the neoplastic cells induce and in which they are dispersed.
Tumors that originate from epithelial cells have a basal lamina that separates clumps of tumor cells from stroma. However, the basal lamina is often incomplete, especially at points of tumor invasion. The stroma is juxtaposed between malignant cells and normal host tissues and is essential for tumor growth. The stroma contains nonmalignant supporting tissue and includes connective tissue, blood vessels, and, very often, inflammatory cells. All solid tumors require stroma if they are to grow beyond a minimal size of 1 to 2 mm.
In addition, tumors that are cancerous also have the property of new blood vessel formation. Blood vessels are only one component of tumor stroma. In fact, in many tumors, the bulk of stroma comprises interstitial connective tissue, and blood vessels are only a minor component of the stromal mass. The stroma also contains tissues and cells from blood including water and plasma proteins, together with various types and numbers of inflammatory cells. There are in addition proteoglycans and glycosaminoglycans, interstitial collagens (types I, III, and, to a lesser extent, type V), fibrin, fibronectin, fibroblasts etc.
How to Prevent Cancer
Cancer risk is related to genes and exposure to several environmental toxins. While certain risks are un-changeable (genes for example), some lifestyle factors if modified may help prevent the occurrence of cancer.
Another important measure for prevention of cancer is by knowing one’s own body and being aware of any changes to detect a possible cancer as early as possible.
A healthy lifestyle can lower the risk of certain cancers. This includes several measures like:
Eating a healthy and balanced diet
There is a lot of research on what raises cancer risk and what reduces it, however, no single food or supplement can prevent cancer from developing. Overall, research shows a link between eating certain groups of foods and a reduction in cancer risk.
Healthy diet includes plenty of fruit and vegetables (at least 5 portions a day), plenty of bread, rice, potatoes, pasta and other foods with carbohydrates and especially those with fiber.Eating enough fiber reduces the risk of bowel cancer. Fibre-rich foods include wholegrain pasta, bread, breakfast cereals and rice. Pulses, fruit and vegetables are also good sources of fibre.
There should be some meat, fish, eggs, beans and other non-dairy sources of protein as well as some milk and dairy foods in diet. Although meat is good source of protein, vitamins and minerals, such as iron and zinc, there is evidence that too much of red processed meat can be bad as it may raise risk of bowel cancer. Red meat includes beef, pork and lamb and processed meat includes bacon, sausages, salami and ham. Diet should contain only small amounts of foods and drinks high in fat or sugars.
Diet should be high in foods with antioxidants. However, some of these in high amounts may raise the risk of cancers. For example, Beta-carotene, often found in antioxidant supplements, has been found to increase the risk of lung cancer developing in smokers and people who have been heavily exposed to asbestos at work.
Maintaining a healthy and normal body weight
High body weight, obesity and being overweight raises the risk of several cancers including bowel cancer, pancreas cancer, esophagus cancer, kidney cancer and breast cancer.
Stopping smoking completely
90% of lung cancer cases are related to smoking. It is the single most important preventable factor in prevention of lung cancer. The earlier smoking is stopped the better it is.
Consuming less alcohol
Excessive alcohol consumption is linked to oral cancer, cancer of the voice box (larynx) or pharynx (back of the mouth), bowel cancer (especially in men), liver cancer and breast cancer (in women). Women shouldn't regularly drink more than 2-3 units of alcohol a day, and men shouldn't regularly drink more than 3-4 units a day.
Preventing prolonged exposure of bare skin to the sun
Skin cancers are common among Caucasians who are exposed to the sun’s ultraviolet rays for long durations of time. Some measures include spending time in shade between 11am and 3pm, using sun screen lotions with sun protection factor (SPF) of at least 15, covering up exposed parts of the body with cloths, hats and sunglasses.
All are advised to keep a watch on any moles or freckles that they have. Any changes in these need to be investigated. This could be signs such as the mole getting bigger or begin bleeding etc.
Prevention of sexually transmitted disease by using safe sex measures
This can prevent transmission of Hepatitis C and Human Papilloma Virus (HPV). The former is responsible for liver cancers while the latter for cervical cancers.
Prevention of exposure to environmental factors
Work place safety among those who work with radiation and with asbestos is important. Exposure to radiation and chemicals like benzene may cause leukemias while exposure to asbestos fibers may lead to lung cancers like mesothelioma.
Drugs for prevention of cancer
Some trials have shown success in this respect. Daily use of tamoxifen, a selective estrogen receptor modulator (SERM), typically for 5 years, has been demonstrated to reduce the risk of developing breast cancer in high-risk women by about 50%. Raloxifene is a SERM like tamoxifen; it has been shown (in the STAR trial) to reduce the risk of breast cancer in high-risk women equally as well as tamoxifen.
Vaccines for cancer prevention
Vaccines against HPV and Hepatits B are available. These can protect against cervical cancer (against HPV – Gardasil and Cervarix) and liver cancers.
Screening
Cancer screening is an attempt to detect unsuspected cancers in an asymptomatic population. These are applied to healthy individuals usually after a certain age. Screening for cancer can lead to earlier diagnosis in specific cases. Early diagnosis may lead to extended life.
Best examples of benefits due to screening include screening for breast cancer by mammograms, for colon cancers through fecal occult blood testing and colonoscopy and for cervical cancers through regular Pap smears for cervical cytology.
Genetic testing
Genetic testing for high-risk individuals is already available for certain cancer-related genetic mutations. Some cancers are typified by certain genetic features. This includes examples like BRCA1 and BRCA2 genes for breast ovarian and pancreatic cancers MLH1, MSH2, MSH6, PMS1, PMS2 for colon, uterus, small bowel, stomach and urinary tract cancers.
Cancer Diagnosis
There are several methods of diagnosing cancer. With advances in technologies that understand cancers better, there is a rise of number of diagnostic tools that can help detect cancers. Once suspected, diagnosis is usually made by pathologists and oncopathologists and imaging radiologists.
Some types of cancer, particularly lymphomas, can be hard to classify, even for an expert. Most cancers need a second opinion regarding diagnosis before being sure of the diagnosis or stage and type.
The most common diagnostic methods include:
Biopsy
This is a test where a small sample of tissue is taken from the suspected cancer with the help of a fine tipped needle (fine needle aspiration – FNA), or with a thicker hollow needle (core biopsy) or by surgical excision. The tissues are then examined under a microscope for the presence of cancer cells. Depending on tumor location, some biopsies can be done on an outpatient basis with only local anesthesia.
Sentinel node biopsy
This is a procedure where the closest and most important nodes near the cancer are surgically excised and examined. Since sentinel nodes are the first location that cancer is likely to spread, only these lymph nodes that likely contain cancer cells.
Endoscopy
In this imaging technique a thin, flexible tube with a tiny camera on the end is inserted into the body cavities. This allows the doctors to view the suspicious area. There are many types of scopes, each designed to view particular areas of the body. For example, a colonoscope looks at the colon and large intestine and a laparoscope is used to look within the abdomen etc.
Blood Tests
Blood tests can be performed to detect the normal blood cells as well as for specific tumor markers. Some tumors release substances called tumor markers, which can be detected in the blood. A blood test for prostate cancer determines the amount of prostate specific antigen (PSA). Higher than normal PSA levels can indicate cancer. Similarly in ovarian cancer a tumor marker CA-125 is released.
Bone marrow aspiration
These show a picture of the bone marrow that may be affected in leukemias and blood cancers.
Pap test
Pap test (Pap smear) is a routine test where a sample of cells from a woman’s cervix is examined under the microscope. This helps identify changes in the cells that could indicate cervical cancer or other conditions.
Sputum analysis and bronchial washing analysis
The cells of the sputum and bronchial secretions are analyzed under the microscope for signs of lung and other respiratory cancers.
Imaging studies
There are several imaging techniques. These include X rays, CT scans, MRI scans of various parts of the body.X-rays are the most common imaging techniques and they may be made more specific by using a Barious enema. This is used for detection of stomach and small intestinal growths and cancers.
Mammogram is an X-ray of the breasts used to screen for and/or detect breast lumps and growths.
A CAT scan (computerized axial tomography) uses radiographic beams to create detailed computerized pictures. It is more precise than a standard X-ray.
An Magnetic Resonance Imaging (MRI) uses a powerful magnetic field to create detailed computer images of the body’s soft tissue, large blood vessels and major organs. Both CT scan and MRI can also be used with contrast radio-labelled dyes to obtain a more clear and specific picture of the cancer.
An Ultrasound uses high-frequency sound waves to determine if a suspicious lump is solid or fluid. These sound waves are transmitted into the body and converted into a computerized image.
Bone scan is specifically used to identify and locate new areas of cancer spread to the bone. Normally a Positron imaging test (PET scan) is used. A Gallium scan is another nuclear medicine test in which a special camera takes pictures of tissues of the body after a special radioactive tracer is injected into a vein. The cancerous areas light up under the scanner.
Genetic analysis
Cytogenetic analysis involves analysis of blood or bone marrow cells for organizations of chromosomes. This shows up any genetic mutations.
Cancer Management
Since there are numerous types of cancer affecting several organs, treatment also differs. Some of the treatment modalities like surgery, radiation therapy, chemotherapy with anticancer drugs are common for nearly all types of cancers.
Some of the types of therapy for cancers include:
Surgery
Surgery is used for initial diagnosis of cancer as well. Sometimes a solid lump or tumor is removed surgically and tissues are examined under the microscope for cancer. This is both a diagnostic and therapeutic use of surgery. Most people with cancer will have some type of surgery. If the cancer has not spread to other organs and tissues, surgery usually helps increase chances of survival to a great extent.
Chemotherapy
Chemotherapy is also called chemo. Despite most diseases being treated by chemicals or drugs, it is cancer therapy with drugs that is termed chemotherapy.These anticancer drugs are cyto-toxic. This means they kill all rapidly growing cells of the body including cancer cells. This also means that chemotherapeutic drugs affect healthy fast growing cells like bone marrow cells, cells that line the gastrointestinal tract and hair follicle cells. When this happens there is bone marrow suppression and decrease in production of red blood cells, white blood cells and platelets in blood. This may lead to anemia, propensity to catch life threatening infections and bleeding tendencies respectively.
When chemo drugs affect the cells of the gastrointestinal tract there may be mouth sores, diarrhea, nausea and vomiting. Due to suppression of hair follicle cells there may be loss of hair or alopecia.Not all anticancer drugs cause these side effects. Some may be fairly selective for cancer cells alone.
Radiation Therapy
After surgery, sometimes radiation therapy is advised. In this therapeutic modality high energy radiation beams are projected on cancerous regions. This kills the cancer cells.
Radiation may be external when the patient needs to visit the hospital for radiation sessions that may last from 10 to 30 minutes.Radiation therapy may also be given internally when small pellets of seeds that emit radiation are implanted in the body of the patient. The seeds emit small amounts of radiation.
Radiation therapy has several side effects including skin burns, changes, fatigue, hoarseness of voice and risk of secondary cancers (this is seen in patients who have had chest radiation who may be at a higher risk of developing breast cancer later in life).
Targeted Therapy
Some types of cancers have specific targeted therapy that affects only the cancer cells and spares the healthy cells. These have significantly lower side effects compared to generalized anti-cancer drugs.
Immunotherapy
This includes therapy with molecules called monoclonal antibodies that target the cancer specifically and spare healthy cells.
Hormonal therapy
Some cancers like breast cancer and prostate cancer are responsive to certain female hormones like estrogen and male hormones like testosterone. Drugs that modulate levels of these hormones are used in therapy of these cancers.
Biological therapy
This includes monoclonal antibodies as well as use of gene therapy and certain vaccines in treatment of cancers.
Stem Cell Transplant (Peripheral Blood, Bone Marrow, and Cord Blood Transplants)
There are several methods of bone marrow transplants that may benefit patients with leukaemia and lymphomas.
Photodynamic Therapy
This therapy involves use of special drugs that are called photosensitizing agents and these are used along with laser light to kill cancer cells. The drugs only work after they have been activated with light.
Cancer Prognosis
Prognosis of any disease means the estimate of the likely course and outcome of the disease. Prognosis of cancers usually means the estimate of success with treatment and chances of recovery.
Factors that affect prognosis of cancer
There are several factors that affect the prognosis of a cancer. Some of these include:
· Type of cancer - some cancers generally have a good prognosis while others are known to be aggressive and come with a high fatality rate
· Location of cancer
· Stage of the cancer – at early stages the prognosis of a cancer is good while at later stages and when the cancer has spread to other organs, the prognosis is usually poor
· Cancer’s grade – a poorly differentiated cancer or a high grade cancer usually carries a poor prognosis
· Patient’s age and general health condition at the beginning of therapy usually determines prognosis to some extent. Newborns and frail elderly individuals usually have a lower chance of surviving the cancer for long and have a poor prognosis.
· Responses to treatment – some cancers are genetically programmed in such a way that they fail to respond to therapy. These carry a poor prognosis.
How is prognosis depicted and explained to the patient?
After considering the factors that affect prognosis the estimated five year survival is calculated for an individual patient. This included all factors like available treatment options, other health problems that can affect successful treatment of the disease. The estimation is determined from information researchers have collected over many years about hundreds or even thousands of people with the same type of cancer.
Some common numbers that are used to determine prognosis include cancer specific survival, relative survival, overall survival, disease-free survival etc. Cancer-specific survival calculates the percentage of patients with a specific type and stage of cancer who have survived their cancer during a certain period of time (1 year, 2 years, 5 years, etc.) after diagnosis. This also called disease-specific survival.
Relative survival is a comparison of survival of patients diagnosed with cancer to survival of people in the general population who are the same age, race, and sex and who do not have that cancer.
Overall survival is the percentage of patients with a specific type and stage of cancer who are still alive during a certain period of time after diagnosis.
Disease-free survival is the percentage of patients who have no evidence of cancer during a certain period of time after treatment. This is also termed progression free survival or recurrence free survival. Usually the common period of time used for these statistics is 5 years.
Why is knowledge of the prognosis important?
Most cancer patients want to know their prognosis. It is easier for many to cope with the diagnosis if they know the possible prognosis of their condition. This also helps patients and their loved ones make decisions regarding possible modalities of treatment, palliative care, and personal matters, such as financial matters and inheritance.
Knowledge of prognosis is the patient’s prerogative. He or she might want to know it or might refuse to know the prognosis of their cancer as they may find it frightening or confusing.
Cancer Epidemiology
Cancers kill thousands of people worldwide. In the United States, for example, cancers form 25% of all deaths. It is also a major health problem in many parts of the world. In the developed world, one in three people will develop cancer during their lifetimes. Cancer can also occur in young children and adolescents, but it is rare. Among children, leukemia is the commonest cancer and the next common cancer in children is brain cancers (notably neuroblastoma).
Furthermore around one third of cancers worldwide are due to potentially modifiable risk factors, which are headed by tobacco smoking, alcohol use, and diets low in fruit and vegetables. In addition, being obese and having a sexually transmitted infection are also risk factors for cancers.
Cancer Research
Cancer is a complex disorder with various manifestations and pathologies at the molecular level. Because of the deadly nature of the disease and its widespread incidence and prevalence, there is intense scientific effort to understand disease processes and discover possible therapies.With the advent of molecular biology and cellular biology and pathological techniques there is a much deeper understanding of the disease compared to a few decades ago.
Incidence, survival and cure rates
Although incidence rates of the disease has risen in most countries, with advent of better therapies survival has lengthened, cure rates have increased and death rates due to cancer decreased dramatically over the last two decades. In the United States a five percent decrease in the cancer death rate (adjusting for size and age of the population) is seen between 1950 and 2005.
Research areas
Molecular basis of cancers
Several factors like immunological and hormonal factors as well cellular signalling molecules have been and are still being studied. These may also provided targets for therapy.
Better screening methods
Better and more cost effective as well as more acceptable screening methods for common cancers are being studied in large populations. Researchers are looking at new methods by which to reduce false positive results (that detect a disease when it is not present) and false negative results (that miss out a cancer or disease when it is actually present).
Better diagnostic tests
Better and more accurate genetic testing and use of molecular biology tools for diagnosis of cancers are being studied and developed. The idea is to bring these techniques to the bed side and make them easily and cost-effectively available to the patients.
Cancer therapy is fraught with fears and risks of side effects. Research is continuously on to find methods that treat and cure the cancer without severely debilitating the patient.
Better cancer prevention and early detection awareness
Research not only focuses on prevention and treatment but also improving awareness regarding better lifestyle measures and early detection of cancers to improve detection, chances of therapeutic success and survival. Research also focuses of several foods and supplements that may help prevent cancers. Researchers are working towards better ways to provide emotional support to cope with cancers. Although, the researcher did not find the long term solutions of it.
In Nepal, we engaged in research from early 2003 and involved curing all types of cancer through Herbs by Nepalese traditional methods and get tremendous success to eliminate cancer.
Related With
Contact Us
Nepal Cancer Cure & Herbs
Research Pvt.Ltd
Dillibazar Pipalbot, Kathmandu, NepalContcat No:-
Mobile No:- 9841522174, 9808793322
Website:- www.cancercareresearch.com
nepalcancercure@gmail.com